Health Coaching
and Collaborative Care

The Problem
Private practice finds itself in a suffocating environment of rising healthcare costs, an aging population and demands for enhancing demonstrable quality outcomes.
Rising Healthcare Costs
Rising Aging Population
Quality Outcome Demand
Payors are shifting to Value Based Reimbursement.
Physician practices are being forced to respond to these challenging demands.

Our Solutions
Pacific Private Practice Network is dedicated to promoting Physician lead and supervised care of patients with chronic conditions and mental health challenges. Our approach is guided by data, and supported by technology, creating a virtual collaborative care team that addresses clinical, behavioral and social determinants.
Promoting Physician Lead
Supervised
Care
Supported by technology
All of our programs provide value-based reimbursement for participating physician practices.



What We Offer
Health Coaching
Health Coaches have five principle roles.
- Providing self-management support
- Bridging the gap between clinician and patient
- Helping patients navigate the health care system
- Offering emotional support
- Serving as a care continuity link.
Within our health coaching program we provide Remote Patient Monitoring and Chronic Care Management
Typical conditions managed in the Health Coaching Program
- High blood pressure
- Diabetes
- Weight loss or gain
- Heart conditions
- Chronic obstructive pulmonary disease
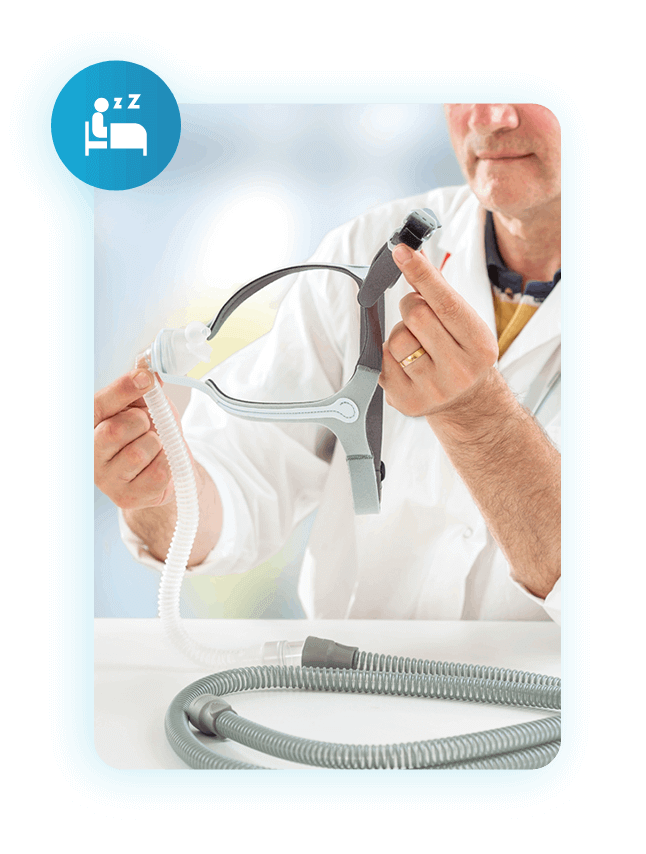
- Sleep apnea
- Chronic insomnia
- Asthma
- Chronic Pain
- Frail elderly
What We Offer
Remote Patient and Therapeutic Monitoring (RPM and RTM)
Remote Patient Monitoring and Remote Therapeutic Monitoring (RPM and RTM) involves the collection and analysis of physiologic data using biometric devices that are used to develop and manage a treatment plan related to chronic conditions. RPM allows physicians to capture data from biometric devices to manage acute and chronic conditions. RTM provides therapeutic patient care delivery and monitoring of musculoskeletal and respiratory conditions, as well as related medication and program adherence.


What We Offer
Chronic Care
Management
What We Offer
Psychiatric
Collaborative Care
Psychiatric Collaborative Care (PsCoCM) is a team-based model of integrated psychiatric and primary care that can treat mental illnesses, such as anxiety, depression, PTSD and substance abuse in the primary care setting. Collaborative Care focuses on defined patient populations tracked in a registry, measurement-based practice and treatment to target. Under primary care supervision behavioral health professionals are embedded into the practice and provide regular evidence-based treatment techniques and medication management. Care is supported by regular psychiatric case consultation and treatment adjustment for patients who are not improving as expected.

What We Offer
Pharmacy Collaborative Care
Pharmacy Collaborative Care (PhrmCoCM) is a contemporary collaborative practice embeds a clinical pharmacist into a team-basedcare model. PhrmCoCM has recently been recognized as a key component of the multidisciplinary approach to health care. Within this model, pharmacists work in collaboration with physicians to provide medication management services.

Pharmacist Responsibilities in PhrmCoCM include:
PHASE I (Initial Activities)
- Prior Authorization Assistance
- Medication Reconciliation, (Indication, Adherence, Safety, Effectiveness)
- Performing follow-up calls post-patient discharge Provide Disease State information, education, and counseling to patients or patients’ caregiver about Medication-related care
- Monitoring Side Effects- notification to physician
- Monitoring response to therapy – notification to physician
PHASE II (Advanced Practice Responsibilities)
- Initiating, modifying, adjusting, discontinuing or monitoring drug therapy
- Ordering, follow up on labs- reporting → adjusting process
What We Offer
Chronic Pain Management
Chronic Pain Management provides a structured chronic pain management program that supports the physician’s practice. The P3N pain team includes a health coach, a pharmacist and a behavioral health professional. The health coach will guide the patient through the program and monitor the patient using validated pain and behavioral health surveys, such as the PHQ9 and GAD7.
Medication management is provided by a pharmacist particularly evaluating adherence, effectiveness, safety and indication. An opioid reduction program is available under the guidance and monitoring of the pharmacist.
Behavioral health managers provide ongoing support using evidence-based techniques including Cognitive Behavioral Therapy, Behavioral Activation, Problem Solving Therapy and Relaxation.

What We Offer
Sleep Disorders
Program
The Value
Influencing patient behavior promotes lifestyle change leading to improved clinical outcomes for patients and healthcare value for payors. Telehealth coaching and collaborative care create an opportunity for structured engagement supported by technology and data to promote and reinforce positive behavior choices. Collaborative care empowers licensed professional such as Health Coaches, Behavioral Care Managers, and Pharmacists, working under the direct supervision of a physician, to provide timely care management and treatment in patients with chronic conditions.


How Are We Different?
We create a care team supporting high risk patients and their caregivers, coordinated by their primary physician who are directly responsible for patient care. We provide real time monitoring using biometric devices, a two-way communication interface between patients, caregivers, their physicians and their care team.
Our coaching approach is built around the principles of behavioral science that creates a conducive environment for change and is refined around descriptive data, supported by ML, and AI to continually influence health coaching interaction and communication. Under the guidance of collaborative care agreements, are empowered to treat patients within their scope of practice under the direct supervision of physicians.
